About Mpox
Mpox has received more publicity in the news recently due to the more virulent Clade I in Africa. Clade I Mpox has NOT been detected in the US at this time. According to Public Health officials, the threat to the general public remain very low. California is monitoring waster data and has not found any evidence of it thus far.
Clade II Mpox (which is endemic to West Africa) caused an ongoing outbreak beginning in 2022 in the United States (and globally). Although the peak of Clade II Mpox had decreased by early 2023, cases continue to be reported at low levels today. Clade II Mpox is considered less severe than Clade I Mpox and more than 99% of people previously infected have survived their infection. Clade II Mpox is less transmissible and usually far less severe than Smallpox as well.
While much lower than in 2022, clade II mpox is still present in the United States. While it's important to stay alert on any emerging public health outbreaks, the current risk of getting clade II mpox in the general public is very low.
Important Announcements
The mpox vaccine (Jynneos) is available for students at Student Health in limited supply through the end of October 2024. After that, Jynneos will become commercially available and there will be a cost for non-UC SHIP insurance. CVS, Rite Aid, and Walgreens in the area now have Mpox vaccines available as well.
JYNNEOS is available to anyone who requests it.
Some factors to consider that may make a person higher risk for mpox are:
- For people aged 18 years and older with the following risks:
- Gay, bisexual, and other men who have sex with men, transgender or nonbinary people who in the past 6 months have had one of the following:
- A new diagnosis of ≥1 sexually transmitted disease
-
More than one sex partner
- Sex at a commercial sex venue
- Sex in association with a large public event in a geographic area where mpox transmission is
occurring
- Sexual partners of people with the risks described above
- People who anticipate experiencing any of the above
- Gay, bisexual, and other men who have sex with men, transgender or nonbinary people who in the past 6 months have had one of the following:
If the above applies to you and you would like to get the vaccine, please login to the patient portal and go to "Appointments" to schedule the mpox vaccine.
Symptoms
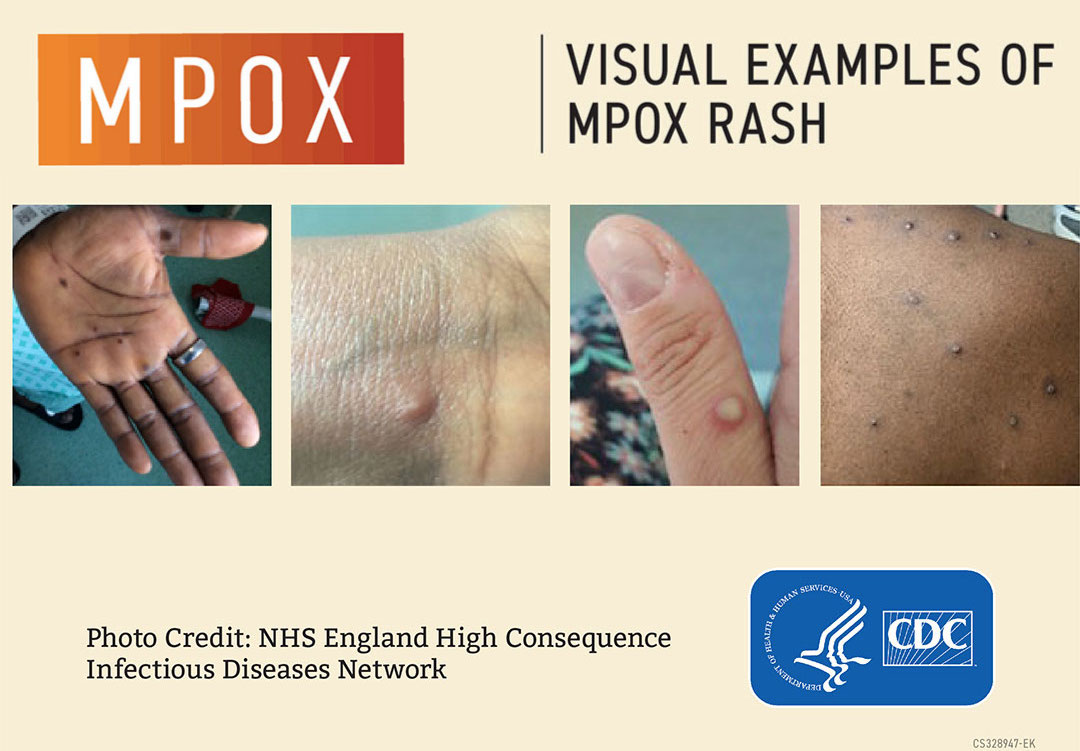
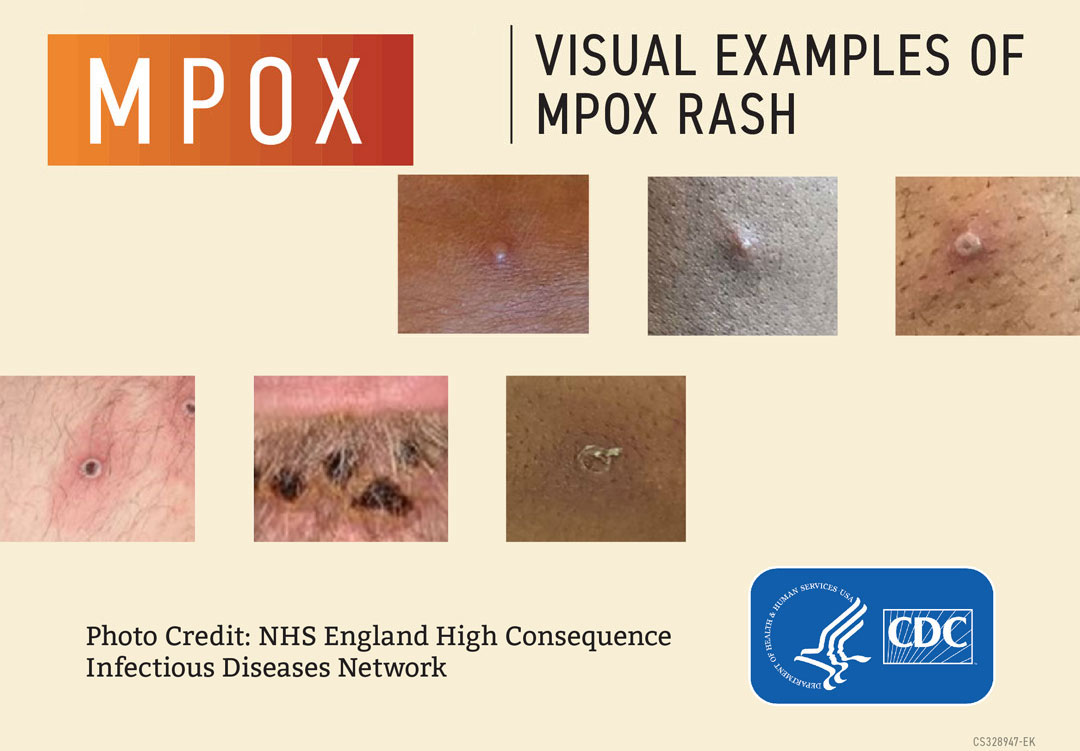
Often, people with mpox will develop a rash or sores on or near the genitals (labia, vagina, testicles, penis) and/or anus (butthole). It can also develop in other regions of the body like the face, mouth, chest, hands, or feet. Sometimes, they might be limited to only one section of the body. The rash/sores can (but not always) be accompanied either before or after with other flu-like symptoms such as:
- Chills
- Fever
- Exhaustion
- Swollen Lymph Nodes
- Muscle Aches or Backache
- Headache
- Respiratory Symptoms like sore throat, nasal congestion, or cough.
For people that experience any flu-like symptoms listed above, rash/sores usually manifest 1-3 days after. Some people only experience a rash and no other symptoms.
Mpox rashes can look similar to common skin conditions. Regular pimples do not warrant concern, but any unusual blemishes or rashes should not be ignored.
The sores will go through several stages, including scabs, before healing. They can look like pimples or blisters and may be painful and itchy. If a person has sores in the anus, bowel movements can be uncomfortable. The illness usually lasts 2-4 weeks.
Mpox can spread from the time symptoms start until all sores have scabbed and fallen off and a fresh layer of skin has formed. This can take several weeks.
Transmission
Mpox spreads in a few different ways. There is a common misconception that mpox can only be spread through sexual contact. While it can be spread through sexual contact, it is not the sole mode of transmission. Here are the primary ways mpox is transmitted:
Skin-to-Skin
Contact
It is primarily through direct skin-to-skin contact with infectious sores, scabs, or body fluids, including (but not only) during sex, as well as activities like kissing, hugging, massaging, and cuddling.
Contact with Porous Materials Used Heavily by A Person with Mpox
Mpox can also spread through touching materials used by a person with mpox that hasn’t been cleaned, such as clothing and bedding. Generally the more porous an object is, the longer it is that the virus may survive on it. However any surface can host the virus, especially in dark, cool, and low humidity conditions.
Respiratory Secretions During Prolonged, Close, Face-to-Face Contact
Kissing or lying next to someone for long periods of time with your faces close together (such as cuddling in very close proximity) can increase the risk of transmission.
To Recap, Mpox Can Be Spread Through:
Non-Sexual Contact
- Direct skin-to-skin contact with rash lesions.
- Living in a house and sharing a bed with someone who is symptomatic.
- Sharing towels or unwashed clothing with someone who is symptomatic.
- Environmental surfaces, particularly when in dark, cool, and low humidity environments.
- Respiratory secretions through prolonged face-to-face interactions (the type that mainly happens when living with someone or caring for someone who has mpox).
Sexual Contact
- Kissing, hugging, massaging, or prolonged face-to-face contact with someone who is symptomatic.
- Touching fabrics and objects during sex that were used by a person with mpox that haven’t been disinfected. This includes bedding, towels, and also sex toys and fetish gear.
- Vaginal, oral, or anal sex where genitals, anus, and/or mouth are in contact with a person with mpox.
- It is UNCLEAR whether mpox can be spread through semen, vaginal fluids, feces, or urine at this time.
Mpox is NOT Spread Through
-
Casual brief conversations.
-
Walking by someone with mpox, such as in a grocery store.
Other Misconceptions
Misconception: Mpox is only spread through sexual contact.
Fact: Mpox is Not Only Spread Through Sexual Contact. It can be spread both through non-sexual contact and sexual contact.
Misconception: Mpox is only a problem for LGBTQIA+ communities.
Fact: Mpox is not limited to LGBTQIA+ communities. Anyone can get it if they are in close contact with a person with mpox regardless of sexual orientation, gender identity, or the sex of one's sexual partner(s). While risk trends may exist at any given point, transmission is not limited to a particular subpopulation.
Misconception: Only men who have sex with men can get mpox.
Fact: Mpox is not limited only to MSM communities (men who have sex with men). Anyone can get it if they are in close contact with a person with mpox regardless of sexual orientation, gender identity, or the sex of one's sexual partner(s). While risk trends may exist at any given point, transmission is not limited to a particular subpopulation.
Exposure Risk
Prevention
There are number of ways to prevent the spread of mpox, including:
- Avoid close skin-to-skin and face-to-face contact, including (but not limited to) sex, with people with symptoms like sores or rashes.
- Avoid contact with materials and objects that a person with mpox has used such as utensils, cups, bedding, towels, and clothing.
- Practicing good hand hygiene. Wash your hands with soap and water often, or use an alcohol-based hand sanitizer. It is especially important to do before eating or touching your face.
- People who become infected should isolate themselves until their symptoms are improving or have gone away completely. The rash should always be well covered until completely healed.
- Using appropriate personal protective equipment (PPE) (like a mask, gown, and gloves) when caring for others with symptoms.
- Always talk to your sexual partner/s about any recent illness and be aware of new or unexplained sores or rashes on your body or your partner’s body, including on the genitals and anus.
- Condoms and Latex Gloves may protect your anus, mouth, penis, vagina, or genitals from exposure. However, condoms alone may not prevent all exposures since the rash can occur on other parts of the body.
- Consider having virtual sex with no in-person contact. Mutual masturbation at a distance apart is safer than skin-to-skin contact sex. Sex with your clothes on over rashes offers more protection than skin-to-skin contact sex as well.
- Avoiding contact with infected materials contaminated with the virus.
- Avoiding contact with infected animals.
What to Do If You Have Had an Exposure or Symptoms
If you’ve been exposed to mpox, call a health care provider or your local health department as soon as you know you’ve been exposed. If you’ve had a high-risk exposure (like from someone you live with or direct contact with a rash/sore), the vaccine should be given within 4 days from exposure to help prevent disease. If given between 4–14 days after exposure, the vaccine may reduce symptoms but may not prevent disease. Monitor for any new symptoms for 21 days after your last exposure. If you develop symptoms, reach out to a health care provider.
Students
Students can make an appointment at Student Health Service through their MyHealth Portal.
Faculty and staff
Faculty and staff should reach out to their primary care provider.
Mpox Home Isolation Guidance for the General Public
For information on isolating at home and returning to public, please click on the following button:
For more up-to-date information on mpox checkout these 3 sites:
CA Dept of Public Health Centers for Disease Control (CDC) SB County Public Health
Vaccines
Student Health Service
JYNNEOS is available to anyone who requests it.
Some factors to consider that may make a person higher risk for mpox are:
- For people aged 18 years and older with the following risks:
- Gay, bisexual, and other men who have sex with men, transgender or nonbinary people who in the past 6 months have had one of the following:
- A new diagnosis of ≥1 sexually transmitted disease
-
More than one sex partner
- Sex at a commercial sex venue
- Sex in association with a large public event in a geographic area where mpox transmission is
occurring
- Sexual partners of people with the risks described above
- People who anticipate experiencing any of the above
- Gay, bisexual, and other men who have sex with men, transgender or nonbinary people who in the past 6 months have had one of the following:
If the above applies to you and you would like to get the vaccine, please login to the patient portal and go to "Appointments" to schedule the mpox vaccine.
Santa Barbara County Public Health
JYNNEOS is available to anyone who requests it.
Some factors to consider that may make a person higher risk for mpox are:
Known close contacts of mpox cases who are identified by public health via case investigation, contact tracing, and risk exposure assessments. (Post-Exposure Prophylaxis (PEP))
- Individuals with certain risk factors who are more likely to have been recently exposed to mpox even if they have not had documented exposure to someone with confirmed mpox, such as people who attended an event or venue where there was known mpox exposure. (Post-Exposure Prophylaxis (PEP)++ )
- Gay or bisexual men and transgender persons 18 years of age and older who have had multiple or anonymous sex partners in the last 14 days including engaging in survival and/or transactional sex (e.g., sex in exchange for shelter, food and other goods and needs)
If you are in one of the categories described above, contact the Santa Barbara County Public Health Department at:
You will be contacted by a Public Health nurse who will ask you about your experience and coordinate your vaccine if indicated.
Please note vaccination criteria will vary by county based on vaccine allocation and current outbreak status.
For More Information About the Vaccine:
FDA JYNNEOS Info CA Dept of Public Health CDC Mpox Vaccine Guidance CDC JYNNEOS Info
UCOP Mpox Info
For more information regarding mpox from UC Office of the President
For inquiries about this website,
please contact:
Jason Stone, M.S.
Health Communication & Media Campaigns Manager
Email: jason.stone@sa.ucsb.edu
Phone: 805-893-4347